Patient experience is increasingly gaining precedence in the healthcare industry as an important part of patient-centric care and is synonymous with patients’ perception of the quality of care received. Today, patient access to medical information through the internet and social media platforms influences how patients perceive care, highlighting the need for the medical community to prioritize patient engagement to improve outcomes. Not only are patients now more educated and informed, but their sphere of influence is also expanding. Further, patient centricity goes beyond the clinical practice setting; it is a priority in the clinical trial setting as well, where the feedback of patients/human participants is essential to evaluate study results. Moreover, patient advocacy groups (PAGs) are exerting their influence on healthcare provider (HCP)-patient interactions as well as clinical trial development, protocols, and data dissemination.
In this article, we will endeavor to capture the global perspective of patient-centric care and patient experience in all the above-mentioned scenarios.
Defining the patient journey
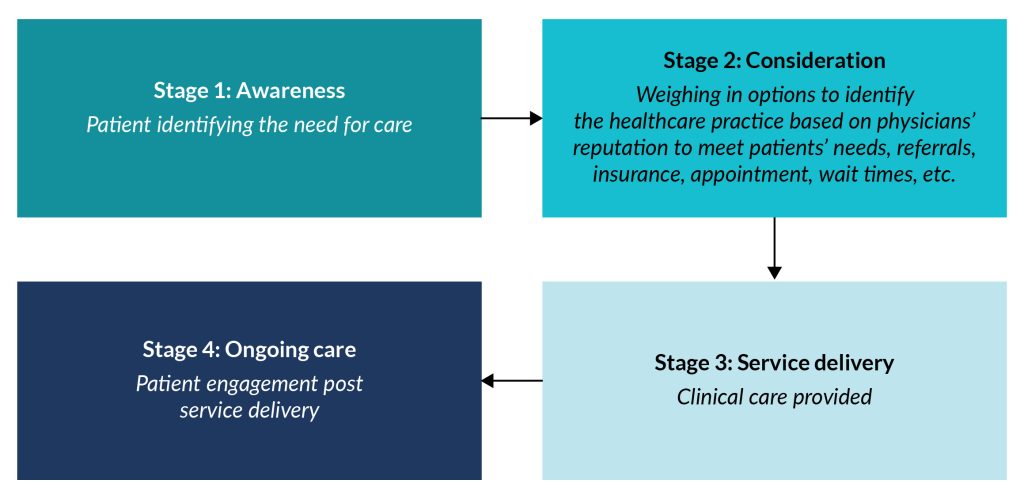
The patient journey covers the course of events that happen at every milestone, from the years preceding the diagnosis of a medical condition to when a patient receives treatment for their condition or to any ongoing care required. Initial steps in the journey include the time point at which a patient first felt the need to seek medical care because of any symptoms experienced, followed by the subsequent outpatient visits until the correct diagnosis. This is followed by identifying and implementing corrective treatment options for clinical care based on the medical condition(s).
Patient experience in a clinical practice setting: Identifying unmet needs to improve care quality
Capturing the complete patient experience during the different stages of the patient journey helps HCPs track the unmet needs associated with delivering quality patient care.
HCPs across countries are striving to provide patient-centric care by not only putting the needs of patients first but also involving them in critical treatment-related decisions. Nevertheless, personalized care received by patients further varies depending on not only the socioeconomic and cultural status of the patients but also on the country they reside in.
Palliative care is another arena wherein wide variations are seen and practiced across the globe. The extent of palliative care received, starting from prescribing pain medication to providing end-of-life care, is governed by local healthcare regulations, policies, and laws. These are often well established in high-income countries, such as the United States and countries in Western Europe. These countries typically have specialized palliative care teams, hospice programs, and dedicated facilities. However, in low- and middle-income countries, access to palliative care may be limited. Incidentally, 78% of adults needing palliative care reside in low- and middle-income countries. Resource constraints, healthcare system challenges, and a shortage of trained professionals could lead to significant gaps in the availability and access to palliative care services. To overcome these variations in care, efforts are being made globally to improve palliative care access and quality through initiatives such as the World Health Organization’s (WHO) public health approach to palliative care.
Leaving aside the legalities, from an individual healthcare practice standpoint, ensuring a positive patient experience starts from the first engagement. From simplifying the appointment process and improving wait times to providing optimal clinical care and post-operative or post-treatment care, the medical community has a multitude of options to choose from for enhancing patient satisfaction in ways that can be captured and measured, including the following:
- The use of digital tools for scheduling appointments, sending reminders, and having provision for online consultations are the first steps toward patient engagement when a patient is in the phase of considering the healthcare practice.
- Providing reliable in-house diagnostic options and accepting multiple insurances and modes of payment help reduce complexities and barriers to access for patients, enhancing efficiencies and increasing consistency.
- Practitioner empathy can improve patient experience during the service delivery phase by encouraging trust and understanding.
- The HCP should be an active listener who can pay attention not just to the signs of the disease that can be objectively detected/measured but also be empathetic toward the symptoms that are subjective and can vary from patient to patient.
- The primary approach of a healthcare practice should not be limited to providing services/amenities but to address the biopsychosocial needs of the patients/primary caregivers in their most vulnerable times.
- Healthcare practices should be forthcoming in providing ample guidance to facilitate informed decision-making by the patient/primary caregiver regarding clinical care. Patient satisfaction substantially increases when they feel connected to their practitioner/physician, which builds trust in the system and has the potential to improve treatment outcomes. Communication being the key, this becomes especially difficult in countries with immigrant population(s). Clinician-immigrant patient interactions are affected when language becomes a barrier.
- Efforts made by the practice/physician to enquire about the patient’s well-being after the culmination of clinical care further positively reinforce patient experience.
- Lastly, seeking patient feedback/reviews on the care received/being received emphasizes the importance of patient-reported satisfaction with the services provided. Objective feedback helps the practice to course correct if needed and improve the quality of care.
Patient experience in a clinical trial setting: The importance of patient feedback/perspectives
In the case of some patients or medical conditions, the existing treatment(s) may not provide benefit, or side effects may interfere with therapy effects. One could argue that patient journey is a two-pronged path; there are patients who are managed successfully and those who are not. This is where clinical trials come in. Clinical trial participation by healthy volunteers and patients with the condition is an integral part of the drug development process. While healthy volunteers participate in a clinical trial to help themselves and others in the future, for some patients, it is their only hope for treatment/cure. Hence, the burden perceived by patients hoping for treatment or cure versus that perceived by healthy volunteers may differ immensely during the study period.
Nevertheless, to improve trial outcomes, it is important to engage all participants holistically in the clinical journey. Incorporating patient centricity starts with clear communication in easily understandable language. Trial participants should be made aware of the potential benefits of the study drug (if it succeeds in the clinical trial) using a fair and balanced approach. Informed consent from patients/participants should be obtained after providing details of the anticipated clinical journey in lay terms. This reduces the number of participants lost to follow-up, as the trial details are well understood prior to the start of the clinical journey, and participants know what to expect. Further, the study design should aim to alleviate patient burden in terms of the number of in-person visits by either conducting completely decentralized clinical trials or including some elements of decentralization as and when possible, such as tele-visits and digital follow-up assessments.
Insights from the participant/patient or caregiver on the clinical outcomes they perceive to be the most important should be considered while the protocol is being developed. Identifying such meaningful outcomes as study efficacy endpoints would augment patient experience and facilitate enhanced regulatory decision-making, including benefit-risk assessments to address patients’ needs. Further, patient-reported outcomes (PROs) in both the clinical trial setting and clinical practice setting are increasingly being considered essential by regulatory bodies and are well on their way to becoming mandatory parts of every clinical trial. The trial outcome should endeavor to improve the quality of life (QoL) of patients rather than just focusing on alleviating signs or symptoms.
Partnership of PAGs in the healthcare industry
PAGs and HCPs work toward the common goal of improving patient journey and treatment outcomes on an ongoing basis. While HCPs provide patients with direct clinical care, PAGs are disease-state experts focused on supporting patients and their families living with a specific disease/condition outside of the medical setting. PAGs exist in most countries; however, they may vary in size, scope, and level of activity. Barring specific functions and activities that might vary among PAGs based on country-specific recommendations, they function worldwide with the common goal of representing the interests of patients.
In addition to raising disease awareness, PAGs are a source of credible information and psychological support to patients and their families. They also play an integral role at the legislative and policy levels, often lobbying to support or oppose policies, regulations, drug approvals, or government funding decisions.
They provide valuable insights during the entire drug development process: from medical research to clinical trial design to regulatory processes to raising awareness and product launch campaigns. PAGs offer training for patient advocates so they can participate more fully in every facet of drug development and are often a conduit for clinical trial recruitment. They are at the forefront of trends such as patient authorship, lay language data dissemination, and brand promotion creative input. By partnering with PAGs, healthcare practices can have access to real-world insights into how to implement patient-centered care and can identify and fill gaps to enhance the overall patient experience from journey initiation onward.
In the absence of patient support groups or PAGs, patients can explore alternative avenues for medical advice and emotional support. These include (i) reaching out to HCPs (doctors, nurses, or psychologists) who may help them connect with appropriate available resources; (ii) online support communities; (iii) local community centers; (iv) online resources and information; (v) national health helplines.
In summary, capturing the patient experience journey in a clinical trial setting or in clinical practice by utilizing first-hand experience—whether individually or via a PAG—is vital to delivering therapies and care that address patients’ real-world concerns in actionable ways and positively reinforce public trust in the healthcare system, resulting in better outcomes. Understanding patient preferences can begin with something as small as how they like to be referred to, for example, putting the person first and not their disability. Ultimately, capturing the patient experience and understanding patients’ needs from a global as well as a local perspective is essential for delivering personalized care and improving outcomes worldwide.
About the author

Swapna Ganduri
Manager, Quality and Training, Cactus Life Sciences.